Lasik Surgery
(Laser In Situ Keratomileusis)
Lasik Overview
(Laser In Situ Keratomileusis)
Earlier operations such as keratomileusis or ALK ( automated lamellar keratoplasty ) created the desired reshaping of the cornea by freezing & lathing the flap or cutting it again with the microkeratome. While effective these operations lacked the precision required for excellent vision in a high percentage of patients. The FDA approval of the excimer made it possible to combine the long established microkeratome techniques with the precise corneal re-shaping of the laser. Thus the LASIK technique was created.
LASIK (Laser In Situ Keratomileusis) is the latest development in a family of procedures known as lamellar refractive surgery. The goal of these operations is to modify the front curvature of the cornea so that light will be properly refracted or focused to achieve a sharp image on the retina. With these surgeries a thin flap of the cornea is lifted using a microkeratome which glides across the cornea like a miniature carpenters plane.
How LASIK Works
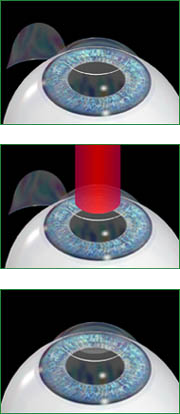
The microkeratome is placed on the eye while the patient is comfortably reclined under the excimer laser.
1. When activated it passes across the cornea lifting a flap just over ¼ of the total corneal thickness.
The flap is gently held to one side and the laser is then centered over the middle of the pupil.
2. While the patient looks at a fixation light the excimer is activated and removes a small amount of cornea in a predetermined pattern, which sculpts it into a new shape.
3. The flap is then repositioned and irrigated to remove any small particles from the eye.
The natural adhesive properties of the cornea allow the flap to remain securely in place without the need for any stitches.
The sculpting of the cornea imparts a new curvature to its front surface thus altering the focal point of the eye to produce a sharp image on the retina. The entire process is completed in 15 – 20 minutes.
Who Can Have LASIK?
LASIK may be used for a fairly wide range of corrections. The FDA has approved the use of an excimer laser to correct nearsightedness up to -14.00 diopters with up to 5 diopters of astigmatism and farsightedness between +0.5 and +5.00 diopters with up to 3 diopters of astigmatism. As the laser is an integral part of LASIK, these become the limits of the procedure. Results have shown that attempted corrections beyond this range may yield less satisfactory visual outcomes. In general patients should be healthy and free of other eye abnormalities. Patients should be at least 21 with a documented stable refraction. Exclusions are listed below:
• corneal diseases including keratoconus or herpes infection of the eye
• vascular illness (i.e. diabetes)
• auto-immune disease (i.e. lupus, rheumatoid arthritis)
• pregnancy
• patients who form excessive scar tissue (keloids)
• patients taking certain medications such as Accutane, Cordarone or Imitrex.
• immunodeficiency
Results with LASIK
The majority of patients who have LASIK are able to achieve unaided vision between 20/20 and 20/40. This is functional vision for most people, permitting all usual activities such as sports, watching television or movies and driving. The initial vision recovery is rapid with much of the improvement already apparent on the first day after the procedure. Some slight fluctuations in vision can take place in the first few weeks. For most patients the results have completely stabilized by six months.
As with any operation unwanted side effects can occur. Either overcorrections or undercorrections are occasionally encountered. In such cases the unaided vision may be somewhat blurry but corrective lenses permit sharp vision. Often a retreatment may be performed to improve the vision. This is generally done after six months to allow for the initial correction to stabilize. Other complications may affect the vision causing it to be blurred even with corrective lenses. Corneal haze associated with healing is rarely seen in LASIK.
However vision may be affected if the flap is damaged. This could occur as an intraoperative problem with the microkeratome or post-op as a result of injury or excessive eye rubbing. It is also possible for particles to become trapped under the flap or for epithelium ( the surface “skin” of the cornea ) to grow under the flap. In the event of a flap problem it may be necessary to perform additional corrective procedures. Fortunately visually significant flap problems are uncommon. Corneal infections or inflammation are rare but can occur. They are usually successfully treated with antibiotic or steroid eye drops.
Custom Laser Treatment
We now have the capability of performing a customized application of the excimer laser to attempt a more complete correction of the elements in the eye’s focusing system that produce blurry vision. This custom approach employs a device called a WaveScan. It is also referred to as wavefront-guided surgery. The concept stems from a technology called adaptive optics which was initially developed to improve the images from astronomical telescopes.
The concept of the WaveScan utilizes an instrument which passes multiple small points of light into the eye and measures the distortion after the light comes back out through all of the focusing elements of the eye. By evaluating how all of these elements have been affected by the eye’s focusing system, a customized map of the eye can be developed. This allows for the evaluation of any irregularity in the eye’s focusing system which may affect vision. In particular, it allows the identification of irregular elements beyond simple nearsightedness and astigmatism which are already correctable by standard laser treatment. The addition of the wavefront-guided technology allows for the possibility of a more accurate correction of the vision. Additionally, because of the way in which the wavefront-guided treatment is applied to the cornea, there may be a better coverage for patients with pupils that dilate to a greater extent in dim light. This therefore can improve the visual performance in low light situations. The application of a wavefront-guided treatment does not produce any significant change in the treatment time or the healing time. It does however require a pre-operative measurement of the eye using the WaveScan device.
Currently, the WaveScan technology is approved in the LASIK platform to correct up to 11 diopters of nearsightedness with up to 3 diopters of astigmatism, as well as up to 3 diopters of farsightedness with up to 2 diopters of astigmatism, and between 1 to 5 diopters of mixed astigmatism. This technology may also be used with the PRK surface treatment for the same indications although this is considered an off-label application according to FDA.
It is important to have detailed discussion regarding whether standard or custom wavefront-guided laser correction would be most appropriate for each individual patient.
Schedule Appointment
to discuss LASIK treatment options